Written by Chris Matich
Humans have used cannabis for pain relief for a thousand years, but only recently have we garnered evidence from controlled, experimental studies regarding its efficacy for treating and helping those with chronic pain.
Chronic pain is extremely prevalent, both in the U.S. and Canada. According to the National Center for Health Statistics, 1 in every 4 Americans suffered from chronic pain in 2006, accounting for 76.2 million people. In their 2011 NCBI report, Schopflocher, Taenzer, & Jovey found that found that 18.6% or just under 6.4 million Canadians suffer from chronic pain.
Finding Relief
Many chronic pain sufferers have begun turning to medical cannabis for relief. In a study evaluating why patients choose medical marijuana and whether these reasons were evidence-based, Kevin Boehnke et al. found that chronic pain made up 62.2% of all patient-reported qualifying conditions.
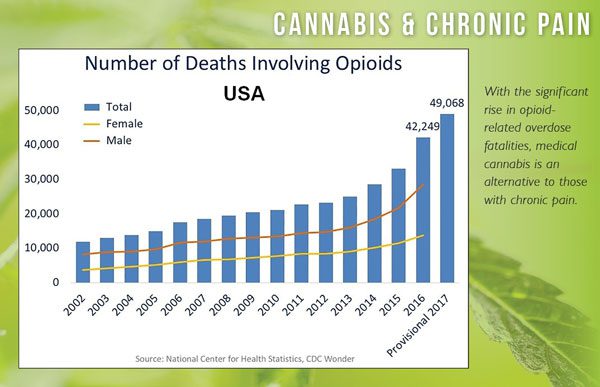
Amid the opioid epidemic, chronic pain sufferers have begun choosing cannabis over traditional narcotics in record numbers. In their 2019 report for the American Pain Society, a group of doctors, led by Boehnke, held an observational analysis of cannabis substitution amongst chronic pain sufferers. Of the 1,321 participants, 80% reported using cannabis for pain relief; 53% from that group made the switch from opioids, leading to speculation that cannabis could help fight opioid addiction. In 2018, Pennsylvania became the first state in the U.S. to offer medical marijuana to those suffering from opioid addiction.
How Cannabis Can Help
We’ve known for quite some time that cannabinoids within the cannabis plant, such as THC and CBD, have healing properties, and in particular a specific efficacy for analgesic relief. In his 2006 literature review, Dr Ethan Russo studied various clinical research regarding approved synthetic forms of cannabis, like Marinol and Nabilone in the U.S., and Sativex in Canada.
Sativex, a cannabis-based medicine with a 1:1 ratio of THC to CBD, became the first ever drug derived from active cannabis to be approved by the FDA in 2018. Russo’s review found that “numerous randomised clinical trials have demonstrated safety and efficacy for Sativex in central and peripheral neuropathic pain.”
Russo also concluded that “cannabinoid analgesics have generally been well tolerated in clinical trials with acceptable adverse event profiles.” While encouraging, Russo’s review concerned what he called, “cannabinoid analgesics,” or the isolated synthetic forms of only one or two of cannabis’ vast array of phytocannabinoids.
So, how do these synthetic, incomplete plant forms compare to smoked cannabis flower? In an experimental study comparing synthetics to natural cannabis, both Marinol and whole plant cannabis showed to be an effective analgesic.
In their 2013 study, Cooper, Comer, & Haney utilised a double-dummy, double-blind procedure to compare the extent of the analgesic benefits daily marijuana and Marinol users experienced using an experimental model of pain. Participants were given the cold pressor test, and their pain sensitivity, tolerance, and subjective experience of pain were recorded.
When compared with a placebo group, participants in both the marijuana and Marinol groups demonstrated decreased pain sensitivity (3.56%; 20 mg), an increased pain tolerance (1.98%; 20 mg), as well as decreased subjective ratings of pain intensity. While Marinol and regular cannabis didn’t differ in terms of pain sensitivity, Marinol produced longer lasting analgesic effects.
So, how does marijuana fight chronic pain on a biological level?
Cannabis And Endorphins
The more researchers discover about marijuana’s many active cannabinoids, the more they learn about cannabis’ pharmacokinetics or the effect the human body has on the drug, and this is no different when it comes to chronic pain. New studies show that pain relieving properties in cannabis can be accredited to its interaction with the endogenous endorphin system.
When marijuana enters the body, it interacts with the endocannabinoid system, or ECS, which serves as a regulatory framework. According to Komorowski & Stepeiń (2007), the ECS produces chemicals that help maintain homeostasis, including those for pain relief.
The ECS is made up of two types of receptors; CB1 and CB2 respectively. You can find these receptors throughout the entire body. They work alongside body-made chemicals to regulate many critical physiological processes. According to Olaizola et al., these include but are not limited to hunger, memory, wakefulness, seizure reduction, and pain sensation.
These chemicals, called endocannabinoids, interact with the CB1 and CB2 receptors. Two of these endocannabinoids, anandamide and 2-Arachidonoylglycerol (2-AG for short), bind and block ECS receptors. They work in sequence as regulators for bodily processes.
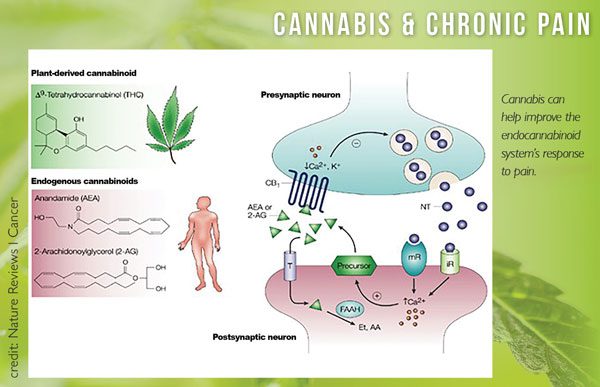
In terms of chronic pain, the ECS releases anandamide, producing feel-good effects similar to that of an endorphin. After a certain amount of time, fatty acid amide hydrolase, or FAAH, gets released into the synapse, as depicted above.
In his 25 year review of endocannabinoid functioning, Mauro Maccarrone (2017) described that FAAH metabolises anandamide, acting as a breaker, switching its feel-good effects on and off. Cannabis chemicals, or cannabinoids, however, may keep anandamide going strong, providing longer lasting analgesic effects.
According to Rodriguez-Murrillo’s 2017 report in CNS Neurol Disord Drug Targets, when cannabinoids like THC and CBD bind to the ECS, some of them block FAAH, keeping it from absorbing anandamide. This extends anandamide’s endorphin-like effects, providing a medical pathway for chronic pain relief that is only a toke away.
A 2018 investigation by Donvito et al. confirmed this potential route of administration, describing that, “cannabinoid receptor agonists as well as inhibitors of endocannabinoid-regulating enzymes fatty acid amide hydrolase and monoacylglycerol lipase produce reliable antinociceptive effects, and offer opioid-sparing antinociceptive effects.”
Ergo, cannabinoids derived from cannabis can help mask nociception, the process by which the body signals pain sensation to the brain. By acting as an antinociceptive, cannabis removes physical awareness of the painful stimulus without the need for harmful opioids.
When you smoke cannabis, chemicals like CBD, THC, and others act upon your endocannabinoid system and increase the action of feel-good chemicals, similar to endorphins; your body’s natural analgesic system. This explains why so many medical marijuana patients use cannabis for chronic pain, and why more studies on chronic pain and medical cannabis are needed in the future.